In IgA Nephropathy
Elevated Proteinuria Increases Risk of Disease Progression1
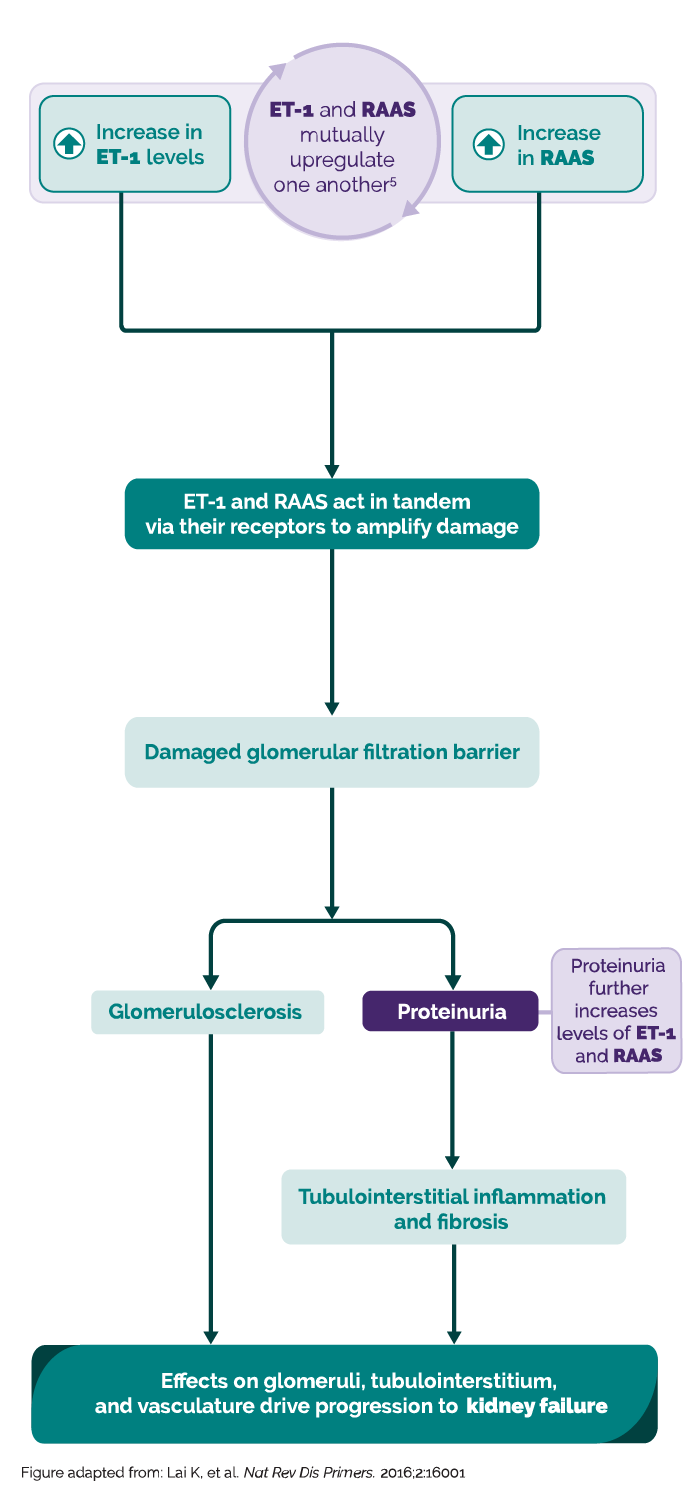
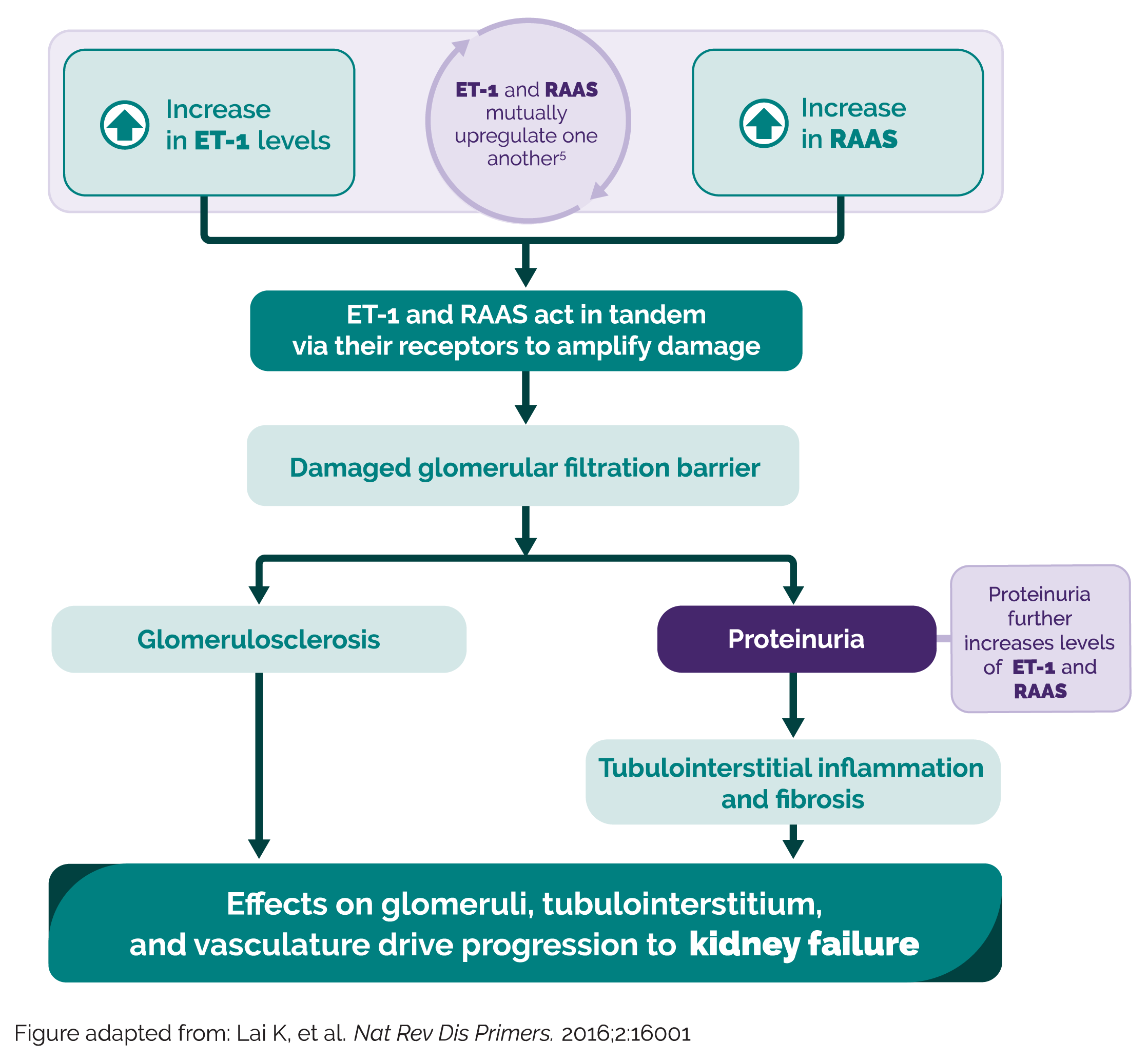
ET-1 and Ang II are two of the key players in driving proteinuria and disease progression in IgAN1-4
The hallmark of IgA nephropathy pathophysiology is the deposition of galactose-deficient IgA containing immune complexes in the mesangium5-7
Persistent proteinuria is the single strongest modifiable prognostic indicator for disease progression in IgA nephropathy8
New data from UK RaDaR analysis provide new insights into disease progression and proteinuria9
Retrospective cohort study – enrollment began in 2013

Patients progressing to kidney failure within 10 years of diagnosisa,b
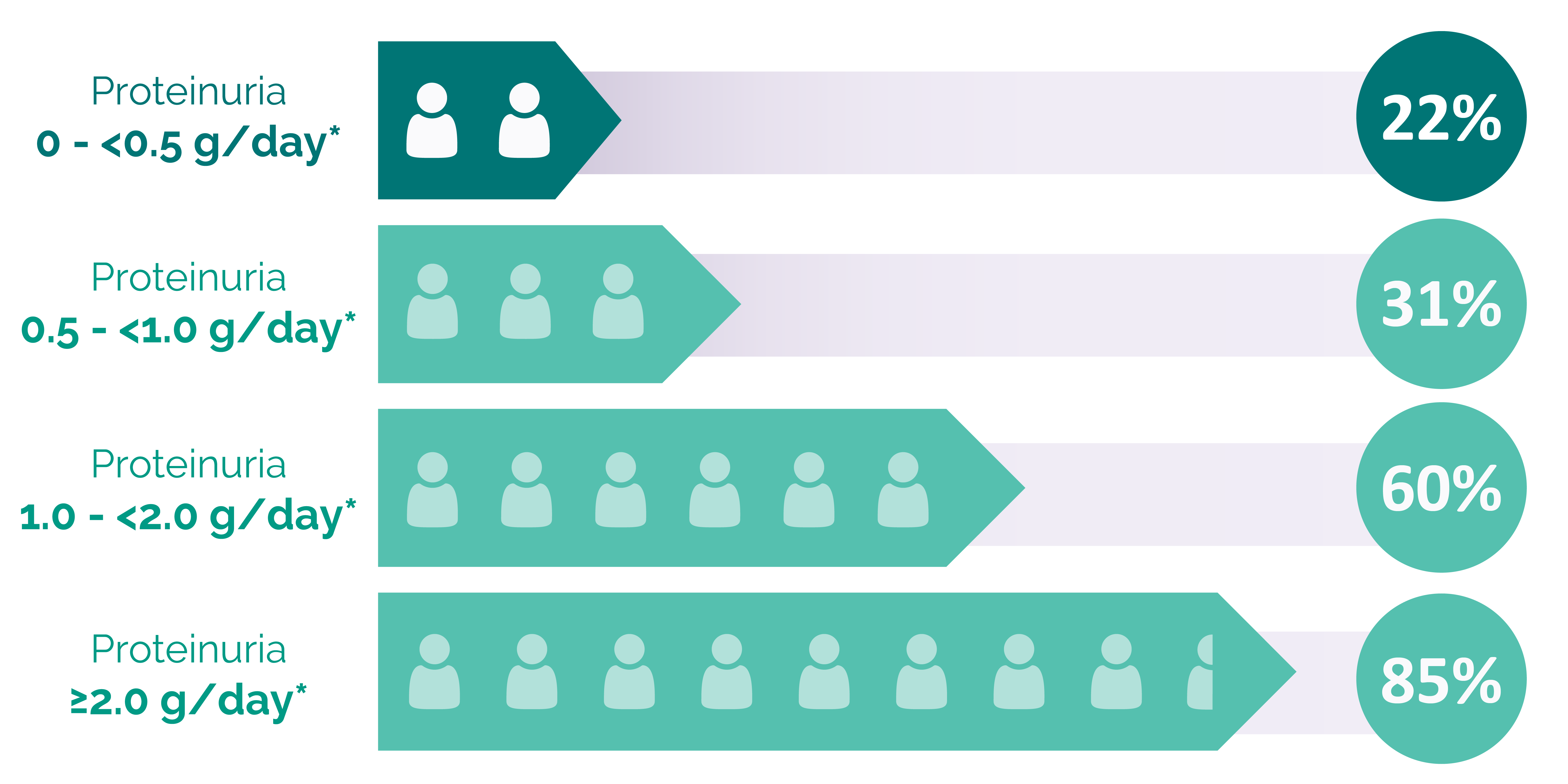
*UPCR 0.88 g/g ≈ 1 g/day.
This analysis received funding from Travere Therapeutics. All instances of proteinuria refer to time-averaged proteinuria, defined as the time-weighted averages for UPCR.
aThe adult patient subpopulation assessed is representative of an incident population, examining time-averaged proteinuria over follow-up without requirement for a baseline UPCR at diagnosis.
bKidney failure defined as the first occurrence of either long-term kidney replacement therapy, a confirmed eGFR <15 mL/min/1.73 m2, or CKD stage 5.
Many patients at proteinuria levels typically perceived as low risk had poor long-term outcomes9
Treatment options historically have been limited.
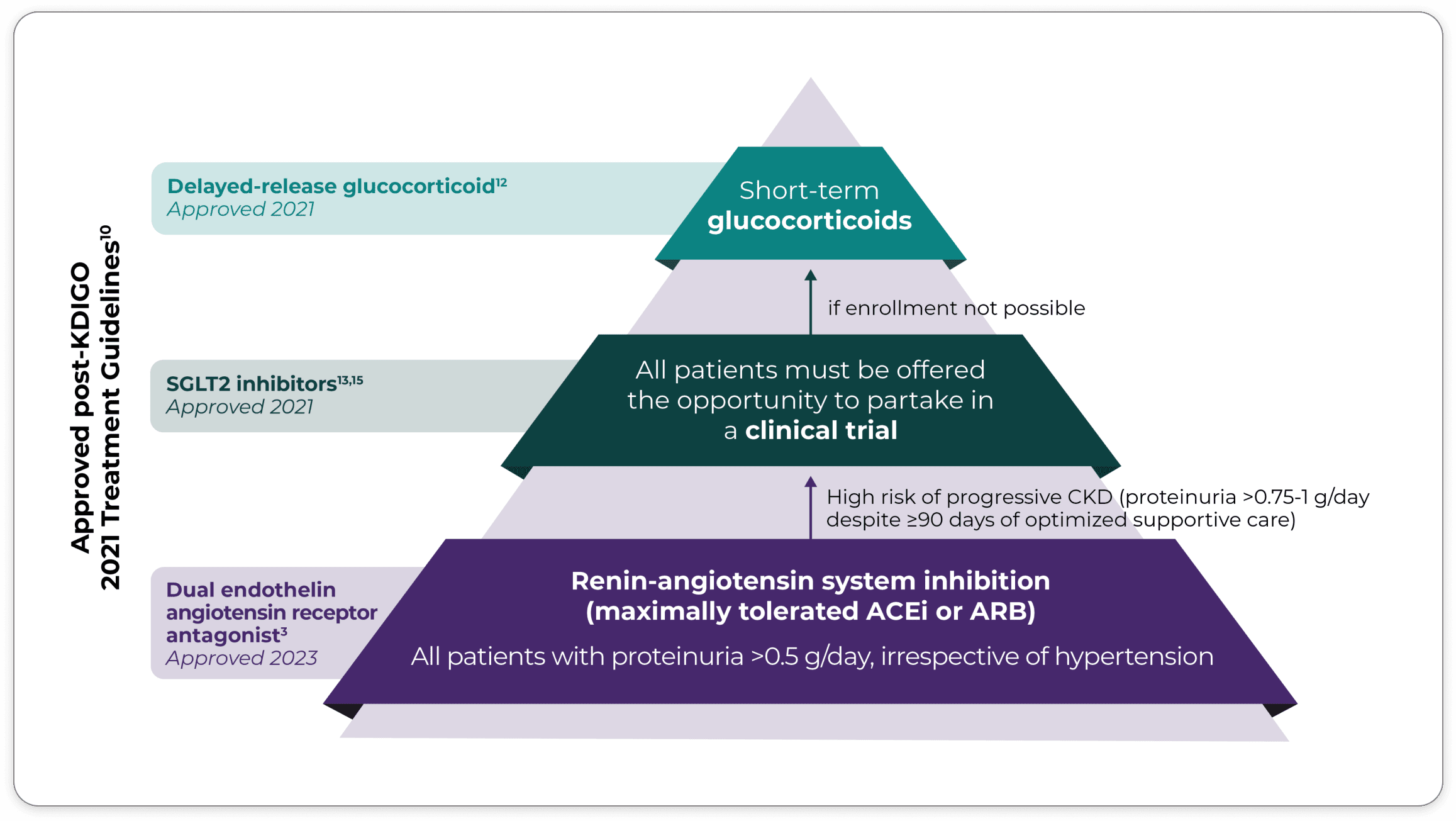
Kidney Disease: Improving Global Outcomes (KDIGO) guidelines 2021 recommend ACEis and ARBs as the current foundational standard of care for IgAN management.10,11*
Expert opinion follows that the KDIGO 2021 guidelines are in need of updating, reflecting the recent advancements in treatment strategies which have been proposed for the management of IgAN. KDIGO guidelines are expected to be updated in 2024.12-14
Recent advancements mean changes in the IgAN treatment landscape: It is time to change the foundational SOC.
Learn about an FDA-approved treatment option for reducing proteinuria in adult patients with IgA nephropathy.
Accurate prognosis leads to optimized patient care
The International Risk-Prediction Tool in IgA Nephropathy†
This simple-to-use tool, based on a risk-prediction model, was developed to assess long-term prognosis in patients with IgA nephropathy16-19:
- An at-biopsy version of the tool was designed for use at the time of biopsy-confirmed diagnosis16
- A post-biopsy version was designed for reassessment of risk at 1 to 2 years after biopsy18
- The tool predicts long-term risk of worsening kidney function, measured as a 50% reduction in eGFR or the development of end-stage kidney disease (ESKD)17,19
- The tool can be run with or without controls for ethnicity (Caucasian, Chinese, or Japanese)16,17,19
- The tool cannot be used to determine the likely impact of any particular treatment regimen10
- The tool incorporates clinical information at the time of biopsy and additional research is needed to determine if the output can be used at other time points in the progression of the disease16
2 ways to access the tool
Download the app:
Calculate by QxMD Mobile App
for iOS and Android devices
Go to the website:
Calculate by QxMD Website
for desktop and mobile browsers
*Multiple other pharmacologic therapies have been evaluated for IgAN, but are not recommended in the guidelines.
†The International Risk-Prediction Tool in IgA Nephropathy was created by QxMD and is not a Travere Therapeutics–sponsored tool.
ACEi=angiotensin-converting enzyme inhibitor; Ang II=angiotensin II; ARB=angiotensin II receptor blocker; CKD=chronic kidney disease; eGFR=estimated glomerular filtration rate; ET-1=endothelin-1; FDA=United States Food and Drug Administration; IgA=immunoglobulin A; IgAN=immunoglobulin A nephropathy; RaDaR=UK National Registry of Rare Kidney Diseases; SGLT2i=sodium-glucose cotransporter-2 inhibitor; SOC=standard of care; UK=United Kingdom; UPCR=urine protein-to-creatinine ratio.
1. Kohan DE, Barton M. Endothelin and endothelin antagonists in chronic kidney disease. Kidney Int. 2014;86(5):896-904. doi:10.1038/ki.2014.143 2. Kohan DE, Rossi NF, Inscho EW, Pollock DM. Regulation of blood pressure and salt homeostasis by endothelin. Physiol Rev. 2011;91(1):1-77. doi:10.1152/physrev.00060.2009 3. Komers R, Plotkin H. Dual inhibition of renin-angiotensin-aldosterone system and endothelin-1 in treatment of chronic kidney disease. Am J Physiol Regul Integr Comp Physiol. 2016;310(10):R877-R884. 4. Raina R, Chauvin A, Chakraborty R, et al. The role of endothelin and endothelin antagonists in chronic kidney disease. Kidney Dis (Basel). 2020;6(1):22-34. 5. Lai KN, Tang SC, Schena FP, et al. IgA nephropathy. Nat Rev Dis Primers. 2016;2:16001. Published 2016 Feb 11. doi:10.1038/nrdp.2016.1 6. Wyatt RJ, Julian BA. IgA nephropathy. N Engl J Med. 2013;368(25):2402-2414. 7. Suzuki H, Kiryluk K, Novak J, et al. The pathophysiology of IgA nephropathy. J Am Soc Nephrol. 2011;22(10):1795-1803. doi:10.1681/ASN.2011050464 8. Reich HN, Troyanov S, Scholey JW, Cattran DC; Toronto Glomerulonephritis Registry. Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol. 2007;18(12):3177-3183. doi:10.1681/ASN.2007050526 9. Pitcher D, Braddon F, Hendry B, et al. Long-term outcomes in IgA nephropathy. Clin J Am Soc Nephrol. 2023;18(6):727-738. doi:10.2215/CJN.0000000000000135 10. Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. Kidney Int. 2021;100(4S):S1-S276. 11. Floege J, Barratt J. IgA nephropathy: a perspective for 2021. Semin Immunopathol. 2021;43(5):625-626. doi:10.1007/s00281-021-00890-9 12. Food and Drug Administration (FDA). FDA approves first drug to decrease protein in IgA nephropathy, a rare kidney disease. https://www.fda.gov/drugs/fda-approves-first-drug-decrease-urine-protein-iga-nephropathy-rare-kidney-disease. Accessed March 2024. 13. Food and Drug Administration (FDA). FDA approves treatment for chronic kidney disease. https://www.fda.gov/news-events/press-announcements/fda-approves-treatment-chronic-kidney-disease. Accessed March 2024. 14. Beck LH Jr, Ayoub I, Caster D, et al. KDOQI US commentary on the 2021 KDIGO clinical practice guideline for the management of glomerular diseases. Am J Kidney Dis. 2023;82(2):121-175. doi:10.1053/j.ajkd.2023.02.003 15. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03762850. Accessed March 2024. 16. Barbour SJ, Coppo R, Zhang H, et al. Evaluating a new international risk-prediction tool in IgA nephropathy [published correction appears in JAMA Intern Med. 2019 Jul 1;179(7):1007]. JAMA Intern Med. 2019;179(7):942-952. doi:10.1001/jamainternmed.2019.0600 17. QxMD IgAN prediction tool for adults at biopsy. https://qxmd.com/calculate/calculator_499/international-igan-prediction-tool-at-biopsy-adults. Accessed March 2024. 18. Barbour SJ, Coppo R, Zhang H, et al. Application of the International IgA Nephropathy Prediction Tool one or two years post-biopsy. Kidney Int. 2022;102(1):160-172. doi:10.1016/j.kint.2022.02.042 19. QxMD IgAN prediction tool for adults post-biopsy. https://qxmd.com/calculate/calculator_839/international-igan-prediction-toolpostbiopsy-adults. Accessed March 2023.
You are about to leave LowerProteinuria.com
Click Continue to leave this site. Click Cancel to remain on LowerProteinuria.com
Cancel